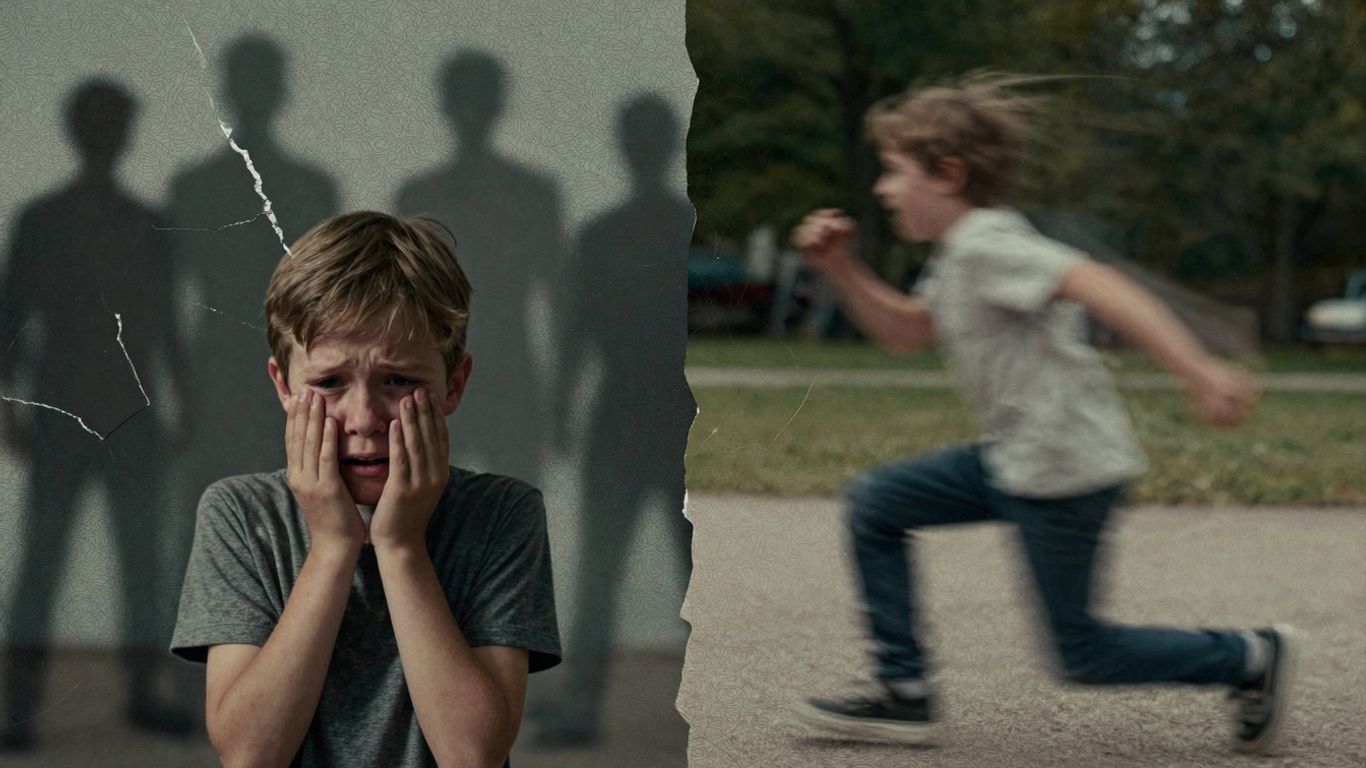
It’s easy to get confused when trying to figure out what’s going on with someone’s behavior. Sometimes, things that look a lot like ADHD can actually be signs of something else entirely, like childhood trauma. This happens more often than you might think, and understanding the connection between childhood trauma and ADHD is super important for getting the right help.
Key Takeaways
- Symptoms of childhood trauma can look a lot like ADHD symptoms, making diagnosis tricky.
- Trauma can affect a developing brain, leading to behaviors that mimic ADHD.
- The relationship between childhood trauma and ADHD is complicated and can work in both directions.
- A thorough assessment is needed to tell the difference between trauma symptoms and ADHD.
- Treating both trauma and ADHD is often necessary for effective support.
Understanding the Overlap Between Childhood Trauma and ADHD
Similarities in Presentation: ADHD vs. Trauma Symptoms
It can get really confusing when trying to figure out if someone’s struggles are due to ADHD or something they went through as a kid. Honestly, they can look a lot alike. Think about it: trouble focusing, feeling restless, or acting without thinking – these are classic ADHD signs, right? But guess what? Kids who’ve experienced trauma often show these exact same behaviors. It’s like they’re wearing the same costume. This overlap makes it tough for parents and even doctors to pinpoint the exact cause. The brain is still developing during childhood, and trauma can really mess with that development, leading to behaviors that mimic ADHD. It’s not always straightforward, and sometimes it feels like a puzzle with missing pieces.
The Complex Interplay: Trauma’s Impact on Developing Brains
When a child goes through something traumatic, especially when their brain is still growing, it can leave a lasting mark. Imagine a young tree that’s been through a harsh storm; it might grow crooked or have weaker branches. Similarly, trauma can affect how a child’s brain wires itself, impacting areas that control attention, emotions, and reactions. This isn’t about blame; it’s about how the brain adapts to survive difficult circumstances. These adaptations, while protective in the moment, can lead to long-term challenges that look a lot like ADHD symptoms. It’s a complex dance between experience and biology.
When Trauma Mimics ADHD: Diagnostic Challenges
Because the symptoms can be so similar, telling the difference between ADHD and trauma-related issues can be a real challenge. A child who can’t sit still might be seen as hyperactive, but maybe they’re actually on edge, constantly scanning their environment for danger because of past experiences. Difficulty concentrating could be a sign of ADHD, or it could be a mind trying to block out intrusive thoughts or memories related to trauma. This is where a careful, thorough assessment is so important. It’s not just about ticking boxes; it’s about understanding the whole picture of a child’s life and experiences. Without this deeper look, a diagnosis might miss the mark, leading to treatments that don’t quite hit the right spot.
Here’s a quick look at some overlapping symptoms:
- Difficulty paying attention
- Restlessness or fidgeting
- Impulsive actions
- Sleep disturbances
- Emotional outbursts
- Trouble with relationships
It’s easy to see how these can be easily confused. The key is to look beyond the surface behavior and explore the underlying reasons.
The Bidirectional Relationship: Trauma and ADHD
How Trauma Can Exacerbate or Trigger ADHD-Like Behaviors
It’s easy to see how trauma and ADHD can get tangled up. Think of it like a really messy ball of yarn – pulling one string can mess up the whole thing. When someone has gone through a tough experience, especially when they were young and their brain was still developing, it can really mess with how they focus, remember things, and manage their emotions. These changes can look a lot like ADHD symptoms. For instance, someone might have trouble concentrating not because of ADHD, but because their mind is busy trying to avoid thinking about something bad that happened. This can lead to what looks like inattention or restlessness, even if the root cause is different.
Does ADHD Increase Vulnerability to Traumatic Experiences?
This is where things get even more complicated. It seems like the relationship can go both ways. People with ADHD might be more likely to end up in situations where trauma can happen. Why? Well, think about the challenges that often come with ADHD: struggling in school, feeling like you don’t quite fit in with others, or getting in trouble for behaviors you can’t easily control. These difficulties can lead to being picked on, feeling isolated, or experiencing more negative interactions with adults. These kinds of experiences, over time, can unfortunately increase a person’s risk of experiencing traumatic events.
The Role of Chronic Stress and Nervous System Dysregulation
When you’re constantly on edge, your body’s stress response system goes into overdrive. This is often called the “fight or flight” response, or sympathetic arousal. It’s your body’s way of saying “danger!” – pumping out adrenaline, making your heart race, and tensing your muscles. For someone with ADHD who might face daily frustrations, criticism, or setbacks, this stress response can become a constant state. The body starts to learn that everything is a threat, even when it’s not. This can lead to physical tension, like clenching your jaw or hunching your shoulders, and a nervous system that’s always on high alert. It’s like the body’s wiring gets rewired, constantly firing in a way that’s meant for emergencies, even in calm situations. This chronic stress and nervous system dysregulation can significantly mimic or worsen symptoms that look like ADHD.
Here’s a look at how chronic stress can affect the body:
- Physical Tension: Muscles may stay tight, leading to headaches or back pain.
- Digestive Issues: The gut is very sensitive to stress, causing problems like nausea or stomach aches.
- Sleep Disturbances: Difficulty falling asleep or staying asleep is common.
- Emotional Reactivity: Increased irritability, anxiety, or feeling overwhelmed.
The constant state of alert that comes with chronic stress can make it incredibly hard to focus on tasks, remember details, or regulate emotions. It’s like trying to read a book in the middle of a fire alarm – your brain is just too busy dealing with the perceived threat to concentrate on anything else.
Navigating Diagnosis: Differentiating Trauma from ADHD
The Difficulty in Distinguishing Core Symptoms
Figuring out if someone’s struggles stem from ADHD or from past trauma can be really tricky. It’s like trying to untangle two very similar-looking threads. Many of the outward signs can look almost identical. For instance, having trouble focusing or remembering things isn’t just an ADHD thing. A mind that’s been through a lot might also struggle to concentrate because it’s busy trying to avoid thinking about upsetting memories. This overlap makes getting the right diagnosis a real challenge. It means doctors and therapists have to look beyond just the surface behaviors.
The Importance of a Comprehensive Assessment
Because the symptoms can be so similar, a quick check-in usually isn’t enough. A thorough evaluation is key. This means taking a good, long look at a person’s whole history, not just their current problems. It involves talking about their childhood, any difficult experiences they’ve had, and how they’ve been feeling and behaving over time. Sometimes, a person might not even realize how a past event is affecting them now, or they might not feel comfortable sharing it right away. Building trust is a big part of this process.
Here’s what a good assessment might include:
- Detailed interviews with the individual.
- Discussions with family members or close friends, if possible and appropriate.
- Review of past medical and psychological records.
- Use of questionnaires and rating scales to gather specific information.
- Observation of behavior in different settings.
Recognizing Trauma-Spectrum Symptoms Beyond PTSD
When we think of trauma, PTSD often comes to mind, but trauma’s effects can show up in many other ways, too. Someone might not have full-blown PTSD but still experience symptoms that look a lot like ADHD. These can include feeling constantly on edge (hypervigilance), being easily startled or jumpy (hyperarousal), having a hard time controlling emotions, feeling numb or disconnected, or experiencing a lot of anxiety and low moods. Physical symptoms like headaches or stomach issues can also be linked to trauma. It’s important for professionals to be aware of this wider range of trauma-spectrum responses when trying to figure out what’s going on.
Impact of Childhood Trauma on Cognitive and Emotional Functioning

Childhood trauma can really mess with how a kid’s brain develops, and it often shows up in ways that look a lot like ADHD. It’s not just about feeling sad or scared; it can actually change how a person thinks and feels on a day-to-day basis. This can make things super tough for kids trying to learn, make friends, or just manage their feelings.
Working Memory Deficits and Trauma-Related Avoidance
It’s interesting how a shaky working memory can be a sign of both ADHD and trauma. With ADHD, it’s often about the brain’s wiring making it hard to hold onto information. But when someone has gone through trauma, their mind might actively try to push away thoughts or memories related to it. This avoidance can look a lot like forgetfulness or an inability to focus on tasks, even though the underlying reason is different. It’s like the brain is trying to protect itself by shutting down certain pathways, which then impacts memory and attention.
Emotional Dysregulation Stemming from Traumatic Experiences
Trauma can leave kids feeling like they’re on an emotional rollercoaster. They might have big, sudden mood swings, get easily overwhelmed by small things, or struggle to calm down once they’re upset. This isn’t because they’re being difficult; it’s a direct result of their nervous system being on high alert for so long. When you’re constantly expecting danger, your emotional responses can become really intense and hard to control. It’s a survival mechanism that gets stuck in overdrive.
Hypervigilance and Hyperarousal as Trauma Responses
Think of hypervigilance as being on constant guard. Kids who have experienced trauma might be super aware of their surroundings, always scanning for threats. This can make them seem jumpy, easily startled, or unable to relax. Hyperarousal is similar; it’s a state of being overly alert and keyed up. Their bodies are ready to fight or flee at any moment, even when there’s no real danger. This constant state of alert drains a lot of energy and makes it really hard to concentrate on anything else.
The brain and body of a child who has experienced trauma can become wired for survival. This means that everyday situations might trigger a strong stress response, making it difficult to regulate emotions, focus attention, or feel safe. It’s a complex reaction that affects many areas of a child’s life.
Here’s a look at how these issues can show up:
- Difficulty concentrating: Trouble focusing in class, on homework, or during conversations.
- Impulsivity: Acting without thinking, which can lead to problems with peers or in school.
- Restlessness: Feeling fidgety or unable to sit still for long periods.
- Emotional outbursts: Intense anger, sadness, or frustration that seems out of proportion to the situation.
- Sleep disturbances: Trouble falling asleep, staying asleep, or experiencing nightmares.
- Physical symptoms: Headaches, stomachaches, or other unexplained physical complaints.
Addressing Co-Occurring Childhood Trauma and ADHD
The Necessity of Treating Both Conditions
When childhood trauma and ADHD show up together, it’s like trying to untangle a really knotted ball of yarn. You can’t just pull one thread and expect everything to straighten out. Treating both conditions is absolutely key to helping someone move forward. Ignoring one can make the other harder to manage, creating a cycle that’s tough to break. It’s not uncommon for symptoms to overlap, making it tricky to figure out what’s what. For instance, that difficulty focusing? It could be ADHD, or it could be a mind trying to avoid painful memories from trauma. This is why a careful approach is needed.
Therapeutic Approaches for Trauma and ADHD
So, what do we do about it? Well, there isn’t a one-size-fits-all answer, but there are several paths that can help. For ADHD, medication can be a tool for some, helping to manage core symptoms like inattention and impulsivity. But it’s not just about pills. Therapy plays a huge role. For trauma, approaches like Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) or Eye Movement Desensitization and Reprocessing (EMDR) can be really effective in processing difficult experiences. When both are present, therapists often integrate strategies. This might mean using behavioral techniques for ADHD symptoms alongside trauma processing. It’s about finding what works for the individual, and often, that means a combination of methods. The goal is to address the nervous system’s response to stress and improve executive functions. Finding the right support can make a big difference in daily functioning.
Support Strategies for Individuals and Families
Beyond formal therapy, there are other ways to offer support. For individuals, learning coping mechanisms is vital. This could involve developing routines, using organizational tools, or practicing mindfulness to manage emotional ups and downs. For families, education is a big part of it. Understanding how trauma and ADHD can interact helps reduce blame and increases empathy. Creating a safe and predictable environment at home can be incredibly beneficial. Sometimes, things like productivity coaching can also be a helpful addition, focusing on practical skills for managing daily tasks.
Here are some general strategies that can be useful:
- Establish Predictable Routines: Consistency helps reduce anxiety and provides structure.
- Practice Mindfulness and Grounding Techniques: These can help manage overwhelming emotions and hyperarousal.
- Encourage Open Communication: Create a space where feelings can be shared without judgment.
- Seek Support Groups: Connecting with others who have similar experiences can reduce feelings of isolation.
It’s important to remember that healing is a process, not a race. Progress might not always be linear, and setbacks are normal. Patience and self-compassion are essential companions on this journey.
The Evolving Understanding of Childhood Trauma and ADHD
Challenging Genetic Assumptions About ADHD
For a long time, ADHD was mostly seen as something you were just born with, a sort of genetic lottery. The idea was that if you had it, it was pretty much set in your DNA. But as we learn more, it’s becoming clear that things aren’t so simple. The environment we grow up in, especially during those early, formative years, plays a much bigger role than we used to think. Think about it: if a child experiences a lot of stress or scary stuff, their brain is going to react. This reaction can look a lot like ADHD symptoms, even if there isn’t a strong genetic link to ADHD itself. It’s like the brain is trying to cope with a difficult situation, and the outward signs are what we often label as ADHD. This shift in thinking means we need to look beyond just genes when we’re trying to figure out why someone is struggling with focus or impulsivity.
The Influence of Environmental Factors on Neurodevelopment
When we talk about environmental factors, we’re really talking about everything that happens around a child as they grow. This includes the stability of their home life, the quality of their relationships, and whether they’ve been exposed to anything upsetting or dangerous. Childhood trauma, whether it’s big events or ongoing difficult situations, can really mess with how a young brain develops. It’s not just about emotional scars; it can actually change how the brain is wired. This can lead to difficulties with things like paying attention, controlling impulses, and managing emotions – all things that are also hallmarks of ADHD. So, a child who has experienced trauma might show behaviors that look a lot like ADHD, not because they have ADHD, but because their brain is responding to a stressful environment. It’s a complex dance between nature and nurture, and the environment can definitely tip the scales.
Future Directions in Research and Clinical Practice
So, where do we go from here? Well, researchers are starting to look more closely at how trauma and ADHD overlap. Instead of just treating ADHD symptoms, clinicians are beginning to ask more questions about a person’s history, especially their childhood experiences. This means that when someone comes in with attention problems, they might get screened for trauma too. The goal is to get a clearer picture of what’s really going on.
Here’s what this evolving understanding means:
- Better Assessments: Doctors and therapists are developing ways to tell the difference between ADHD symptoms and trauma responses. This involves asking more detailed questions and looking at the whole person, not just isolated behaviors.
- Tailored Treatments: If trauma is a big part of the picture, treatments will need to address that directly, often alongside ADHD strategies. This might involve therapy focused on processing difficult experiences.
- Less Stigma: By understanding that certain behaviors might stem from trauma, we can reduce the stigma associated with conditions like ADHD. It helps people realize they aren’t
Moving Forward: Understanding and Support
It’s pretty clear that the line between ADHD symptoms and the effects of childhood trauma can get really blurry. Sometimes they look so much alike, it’s hard to tell them apart, and often, one can make the other worse. The important thing to remember is that no matter the root cause, whether it’s ADHD, trauma, or a mix of both, getting help is key. Recognizing these overlaps is the first step. It means we need to look at the whole picture when someone is struggling, not just check boxes for a diagnosis. Finding the right support, whether that’s therapy, coaching, or other resources, can make a huge difference in helping people manage their symptoms and live better lives. It’s about acknowledging the complexity and offering compassionate, effective care.
Frequently Asked Questions
Can childhood trauma look like ADHD?
Yes, it really can! Sometimes, the way a child acts after going through a tough experience can seem a lot like ADHD. Things like having trouble focusing, being jumpy, or acting without thinking can happen with both trauma and ADHD. It’s like they’re wearing similar masks, making it tricky to tell them apart.
Does trauma cause ADHD?
It’s not that simple. While trauma doesn’t directly cause ADHD, it can make ADHD symptoms appear or get worse. Think of it like this: someone might have a tendency towards ADHD, and then experiencing trauma makes those tendencies much more obvious. The relationship is complicated, and sometimes it’s hard to know which came first or if they’re just tangled together.
Why is it hard to tell the difference between ADHD and trauma symptoms?
It’s hard because they share many of the same signs. For example, both can make it tough to pay attention, remember things, or control emotions. When a child has been through something traumatic, their brain and body are on high alert, which can look a lot like the restlessness and impulsivity seen in ADHD. Doctors need to look very carefully at a person’s whole story to figure it out.
Can having ADHD make someone more likely to experience trauma?
It’s possible. People with ADHD might sometimes struggle with social situations or be more impulsive, which could put them in situations where they are more vulnerable to experiencing upsetting events. Also, if someone is having a hard time focusing or controlling their actions, they might face more difficulties in school or with others, which can lead to stressful experiences.
What happens to the brain when someone experiences trauma?
When someone goes through trauma, especially when they are young, their brain can get stuck in a ‘danger’ mode. This is called the ‘fight or flight’ response, and it can stay activated. This constant alert can make it hard to relax, focus, and manage feelings, similar to how ADHD affects the brain. It’s like the body’s alarm system is always on.
How should someone be treated if they have both trauma and ADHD?
It’s really important to treat both conditions. Usually, this means getting help for the trauma first, often through therapy that focuses on healing from difficult experiences. Once the trauma is being addressed, treatments for ADHD, like therapy or sometimes medication, can be more effective. The goal is to help the person feel safe and learn skills to manage both challenges.
